Allergies
Allergic diseases, including allergic rhinitis, atopic dermatitis, food allergy, and asthma, are the most common chronic immune-mediated diseases that affect children and adults with increasing prevalence worldwide.1 They are defined by an excessive or unnecessary immune response to an innocuous environmental allergen, manifesting in various undesirable and potentially life-threatening symptoms, including anaphylactic shock.2
Immune Response
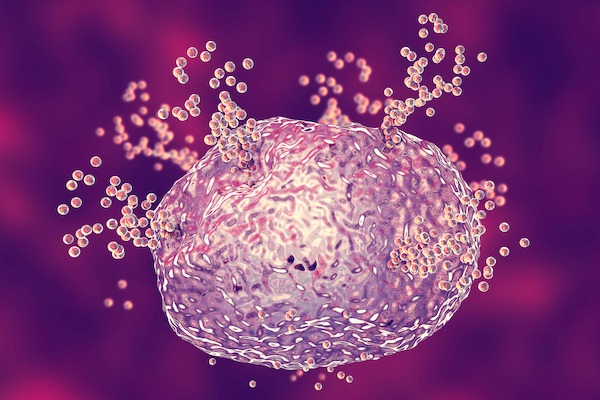
Genetic, developmental, and environmental factors all play crucial roles in the pathogenesis of allergic diseases, with epigenetic modifications mediating the effects of allergen exposure and the resulting outcome.1 Allergic reactions can be characterized by their immunological mechanisms as either IgE mediated or non-IgE mediated reactions. IgE-mediated allergic diseases are the most common, and begin with a sensitization phase where the individual develops an immune memory to a specific antigen:3
- Sensitization – allergens that enter the body during initial exposure are captured, digested into peptide fragments, and displayed by antigen-presenting cells (APCs). Circulating T cells then interact with APCs, initiating the expression of Th2 cytokines and inducing B cells to produce IgE antibodies. These allergen-specific IgE antibodies then bind to mast cells and basophils.4
- Re-exposure – the allergen will bind to the surface IgE, causing rapid degranulation of mast cells or basophils, resulting in the release of inflammatory compounds – such as histamine – and the influx of inflammatory cells.5
Sources and Strategies for Treatment
There are various medications to manage the symptoms of an allergic reaction, including antihistamines, decongestants, and corticosteroids. Allergen immunotherapy (AIT) is an effective long-term treatment based on the controlled and repeated exposure of a patient to an allergen which, over time, lessens their body’s immune response.6 The European Academy of Allergy and Clinical Immunology (EAACI) and the World Allergy Organization (WAO) provide guidelines and evidence-based recommendations for managing different IgE-mediated allergies with various methods of AIT.7, 8
The past decade has witnessed the development of AIT drugs that operate through various mechanisms, including the desensitization of early mast cells and basophils, the regulation of T and B cell responses or IgE production, and the inhibition of immune cell responses in affected tissues.9 These therapies are most commonly administered via injection (subcutaneously) or orally (sublingually), with some studies suggesting that the former can be more effective with certain allergies.10 It is crucial to investigate predictive biomarkers in serum – such as allergen-specific IgE levels or basophil activation – to determine the efficacy of these treatments.6 With prevalence of allergies rising, the attention for AIT is increasing, and researchers and governing bodies are working to standardize the administration of therapies, improve their safety, and prolong the effect of AIT cessation for greater efficacy.11
Related Content
References
1. Akhtari, M., & Mahmoudi, M. (2019). Epigenetic biomarkers of asthma and allergic disorders. In Prognostic Epigenetics (pp. 139-169). Academic Press.
2. Sicherer, S. H. (ed.). (2013). Food allergy: practical diagnosis and management. CRC Press.
3. British Society for Immunology. (2022). Retrieved 24 January 2022, from https://www.immunology.org/policy-and-public-affairs/briefings-and-position-statements/allergy
4. Oettgen, H., & Broide, D. H. (2011). Introduction to mechanisms of allergic. Allergy E-Book, 1.
5. Yu, W., Freeland, D., & Nadeau, K. C. (2016). Food allergy: immune mechanisms, diagnosis and immunotherapy. Nature reviews. Immunology, 16(12), 751–765. https://doi.org/10.1038/nri.2016.111
6. Nakagome, K., & Nagata, M. (2021). Allergen Immunotherapy in Asthma. Pathogens (Basel, Switzerland), 10(11), 1406. https://doi.org/10.3390/pathogens10111406
7. Alvaro-Lozano M, Akdis CA, Akdis M, et al. (2020) EAACI Allergen Immunotherapy User's Guide. Pediatric Allergy and Immunology. 31 Suppl 25(Suppl 25):1-101. doi: 10.1111/pai.13189. PMID: 32436290; PMCID: PMC7317851.
8. Simons, F. E., Ardusso, L. R., Bilò, M. B., El-Gamal, Y. M., Ledford, D. K., Ring, J., Sanchez-Borges, M., Senna, G. E., Sheikh, A., Thong, B. Y., & World Allergy Organization (2011). World allergy organization guidelines for the assessment and management of anaphylaxis. The World Allergy Organization journal, 4(2), 13–37. https://doi.org/10.1097/WOX.0b013e318211496c
9. Berings M, Karaaslan C, Altunbulakli C, Gevaert P, Akdis M, Bachert C, Akdis CA. Advances and highlights in allergen immunotherapy: On the way to sustained clinical and immunologic tolerance. J Allergy Clin Immunol. 2017 Nov;140(5):1250-1267. doi: 10.1016/j.jaci.2017.08.025. Epub 2017 Sep 20. PMID: 28941667.
10. Tsabouri S, Mavroudi A, Feketea G and Guibas GV (2017) Subcutaneous and Sublingual Immunotherapy in Allergic Asthma in Children. Frontiers in Pediatrics. 5:82. doi: 10.3389/fped.2017.00082
11. Pfaar, O, Bousquet, J, Durham, SR, et al. (2021) One hundred and ten years of Allergen Immunotherapy: A journey from empiric observation to evidence. Allergy. 00: 1– 15. https://doi.org/10.1111/all.15023

